In a multi-center study, Dr. Niroj K. Sahoo from LVPEI, Dr. Jay Chhablani from the University of Pittsburg, and others, analyzed the longitudinal changes in eyes with chronic or acute central serous chorioretinopathy to better understand disease progression over time.
Central serous chorioretinopathy (CSCR) is an eye disorder in which fluids accumulate under the retina, the innermost layer of the eye. Leakage from blood vessels in the choroid, a vascular layer surrounding the retina, results in the accumulation of fluid, which then causes parts of the retina to bulge and distort, resulting in blurred vision. Acute CSCR, the common variant, is self-resolving with good visual recovery. Chronic or recurrent CSCR is a rare variant that can permanently damage the retina and the retinal pigment epithelium (RPE), a tissue layer that maintains the retina, and may require treatment.
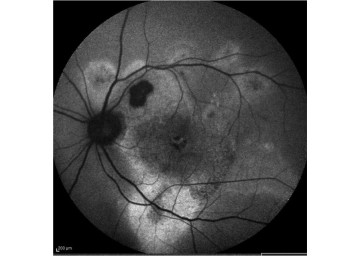
CSCR is marked by several morphological changes to the eye. Apart from fluid accumulation, CSCR is marked by increased choroid thickness (CT), a dysfunctional RPE, changes in the natural fluorescence (autofluorescence) of the retina, and a ‘double layer sign’ (DLS), indicative of abnormal blood vessel formation (neovascularization) in the choroid. While multiple studies confirm these changes in ocular morphology during CSCR, little is known on how these characteristics change with time and how they differ between acute and chronic CSCR. Understanding these changes can shed light on why some people develop a vision impairing deviation to an otherwise self-healing condition.
In a new study published in the European Journal of Ophthalmology, an international team of researchers including Dr. Niroj K. Sahoo from LVPEI, Dr. Jay Chhablani from the University of Pittsburg, and others, analyzed the longitudinal changes in imaging parameters in eyes with chronic or acute CSCR. In an earlier study, the researchers had also evaluated risk factors for chronic CSCR. This longitudinal retrospective study included data from 146 patients (175 eyes) with CSCR and at least four years of follow-up. Among them, 52 eyes had acute, and 123 had chronic CSCR. The researchers used two imaging methods to record longitudinal changes in CSCR: optical coherence tomography (OCT), a non-invasive method of taking cross-sectional images of the retina, and fundus auto-fluorescence (FAF), which captures the RPE health.
The researchers observed a decline in choroidal thickness over time in both acute and chronic CSCR. However, the conditions had some clear differences in presentation. The ‘double layer’ was stable in acute CSCR, but continued to widen in the chronic variant, suggesting the formation of new—and sight-threatening--blood vessels in the choroid. Similarly, the area of RPE alteration varied between the chronic and acute variations of this condition. The researchers also found that a lower central macular thickness and less intraretinal fluid at the onset of CSCR, a characteristic of chronic CSCR, is associated with more RPE dysfunction. The study demonstrates that chronic CSCR often starts with less extreme morphological changes, unlike acute CSCR, but has a wider variety of changes over time. There is a sufficient difference in their presentation to warrant considering them as separate entities.
‘We found that various imaging parameters in acute and chronic CSCR had different rates of progression with minimal overlap, even after long follow-up. This could imply that the nature and severity of these two entities could be different, and not sequential,’ notes Niroj Kumar Sahoo, consultant ophthalmologist at LVPEI’s KVC campus in Vijayawada, and the first author of this paper.
Citation
Sahoo, N. K., Ong, J., Selvam, A., Maltsev, D., Sacconi, R., Venkatesh, R., Reddy, N. G., Madan, S., Tombolini, B., Lima, L. H., Pramil, V., Anantharaman, G., Casella, A. M., Ledesma-Gil, G., Waheed, N., Borrelli, E., Querques, G., & Chhablani, J. (2024). Longitudinal structural changes in central serous chorioretinopathy: A multimodal imaging-based study. European Journal of Ophthalmology, 11206721241287253. Advance online publication. https://doi.org/10.1177/11206721241287253