In a new study, Drs. Soumyava Basu, Shabtab Nasir, and others evaluated the presenting visual acuity, the extent of vision impairment, and risk factors among children with uveitis, when they came to LVPEI.
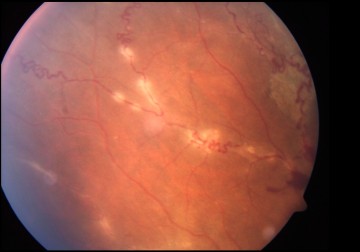
Uveitis is a complex, sight-threatening condition, in which the uveal tissue, which wraps around the ocular tissue, is inflamed. Injury, infection, or even systemic autoimmune triggers can cause the uvea to swell up, resulting in blurred vision or even sight loss. In fact, one in every four cases of blindness in low- and middle-income countries is estimated to be caused by uveitis. Children with uveitis are particularly in danger of losing their sight due to the early onset of the disease and delays in diagnosis. In fact, children with uveitis have a more severe, and a higher chance of sight loss, than adults. They are also at risk of developing secondary eye conditions such as amblyopia (lazy eye), glaucoma, or pediatric cataract.
Studies in high-income countries show that roughly one-third of children with uveitis have severe vision impairment (VI). Some of the underlying causes include cataracts, keratopathies, and glaucoma. One reason behind the prevalence of VI is that childhood uveitis often begins with no symptoms of pain or redness. Vision loss is often the first symptom, and children or their parents are not able to perceive it in the early stages. Apart from presenting visual acuity, every other symptom is confounded by the many complexities in disease pathogenesis and lack of access to treatments. Most studies on uveitis focus on the long-term visual outcomes of the disease rather than visual acuity at presentation. However, VI (as a measure of visual acuity) at presentation can be an effective metric for assessing the need for early intervention and can even be a reference point for tracking changes in uveitis awareness over time.
In a new study published in the journal Ocular Immunology and Inflammation, Drs. Soumyava Basu, Shabtab Nasir, and others from LVPEI, evaluated the extent of VI at presentation among children with uveitis. The study involved a retrospective analysis of the electronic medical records of 477 children with uveitis from four tertiary hospitals of LVPEI, across three Indian states. The patients were on average 11 years of age and most of them (64.8%) had uveitis in both eyes. The severity of VI was determined by the best documented visual acuity of the better eye when they first reported to LVPEI.
All children underwent a complete eye examination, but only 205 (~43%) returned with all the laboratory investigations advised to them. Among them, 32.7% of children had undifferentiated uveitis (uveitis without a clear cause), 31.7% had uveitis due to infections, 25.7% had uveitis in association with juvenile idiopathic arthritis, an autoimmune disease, and 10.2% had another non-infectious uveitis. One-fifth (21%) of the children had moderate-to-severe VI (MSVI). MSVI was primarily seen in older children and in those who had received oral corticosteroids before coming to LVPEI, while female gender, use of topical corticosteroids (suggestive of milder disease), or other immunosuppressive treatment reduced the risk. Cataract, band-shaped keratopathy—an eye disease that causes calcium deposits in the cornea—and retinal detachments were the most common complications observed in the children. This is the largest series of pediatric uveitis from India, and the second largest from anywhere in the world.
'This study highlights the need for raising awareness about pediatric uveitis amongst ophthalmologists, rheumatologists, pediatricians, and the general population,' concludes Dr. Soumyava Basu, Network Head of Uveitis Services at LVPEI and the corresponding author of this paper. 'The findings of this study will help in early diagnosis of the condition and prevent visual impairment.'
Citation
Nasir, S., Ali, M. H., Patel, A., Kelgaonkar, A., Nayak, S., Tyagi, M., Murthy, S., & Basu, S. (2024). Visual Impairment at Presentation in Pediatric Uveitis: A Multicentric Study in 477 Children Across Southern and Eastern India. Ocular Immunology and Inflammation, 1–5. Advance online publication. https://doi.org/10.1080/09273948.2024.2401134