A new study by Drs Sayan Basu, Anahita Kate, and others from the L V Prasad Eye Institute describes the ocular manifestations of chronic Graft vs Host Disease in hematopoietic stem cell transplantees of Indian ethnicity. They have characterized the resultant Dry Eye Disease and the risk factors for a progressive, sight threatening disease.
Persons with disorders of the blood like acute lymphocytic leukaemia, acute myeloid leukaemia, or aplastic anaemia, are indicated for a bone marrow or hematopoietic stem cell transplantation (HSCT), with grafts likely sourced from a donor. Hematopoietic stem cells are precursors to a variety of blood cells, including immune cells. So, a significant percentage of graft recipients may develop serious complications when these grafted immune cells attack the host--their body. Chronic Graft vs Host disease (GvHD) is a systemic condition involving a variety of organs, including the eye.
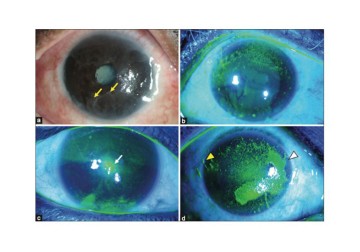
GvHD manifests in the eye as Dry Eye Disease (DED), where the surface of the eye and the conjunctiva—the membrane that lines the eyelids and eye-whites—go ‘dry’. A key test for DED is measuring tears on the ocular surface using the Schirmer’s test. A low Schirmer’s test score points to inadequate tear fluid on the ocular surface. A low score in a person who underwent a hematopoietic stem cell transplant indicates DED, and therefore, also indicates GvHD. GvHD is complex and an ophthalmologist must consider a set of subjective and objective aspects before diagnosing the condition. GvHD’s many manifestations also vary based on ethnicity and lineage. However, most current literature and studies describing the ocular manifestations of GvHD are limited to high-income countries. There is a need to better characterise ocular GvHD in diverse populations across the world.
In a new paper in the Indian Journal of Ophthalmology, Drs Sayan Basu, Anahita Kate, and others from LVPEI address this lacuna by characterising GvHD in an Indian cohort. They report on a retrospective review of case records, of patients with chronic ocular GvHD over a 9-year period (2011-2020). A total of 68 eyes of 34 patients (79% male; 21% female) with a median age of 33 years were included. 6 patients were 18 years old or younger. 65% had ocular GvHD alone, while the rest had other systemic involvement. Nearly 85% of the cases had severe DED with a Schirmer’s test score of less than 5mm. Conjunctival and corneal staining was conducted on all eyes (68) with grading for severity, a measure of ocular surface inflammation.
All patients had no noticeable vision impairment (median of 20/25 or 0.1 LogMAR). However, 32% had a progressive form of the disease with increasing risk of sight loss—the prevalence was similar in paediatric and adult participants. Topical immunosuppression was instituted in nearly 90% of cases with which they showed a significant improvement in the corneal staining scores. However, conjunctival scores showed little improvement despite this therapy over the course of the study and were an important risk factor for a progressive disease. GvHD requires systemic therapy for its control and hence a multi-disciplinary approach is necessary to provide optimal care. The study underscores the need to screen patients for DED prior to a HSCT. These and many other findings in this paper paint a detailed picture of the severity and progression of GvHD particular to an Indian population—a key addition to our knowledge of this condition.
‘This study highlights the importance of regular dry eye screening for patients undergoing bone-marrow transplant. This is necessary for the early diagnosis, treatment, and prevention of corneal complications,’ says Dr Sayan Basu, the Prof. D Balasubramanian Chair of Eye Research at LVPEI.
Dr Anahita Kate, consultant ophthalmologist at LVPEI, and the first author, adds, ‘to ensure proper care, patients undergoing bone-marrow transplants should have regular eye check-ups and there should be more collaboration between ophthalmologists and hemato-oncologists.’
Citation
Kate A, Singh S, Das AV, Basu S. Dry eye disease and risk factors for corneal complications in chronic ocular graft‐versus‐host disease. Indian J Ophthalmol 2023;71:1538‐44.
Photo credit: Fig 2, Chronic ocular graft‐versus‐host disease; Kate et al.