By February 2022, India recorded over 42 million confirmed COVID19 cases. We have been through three ‘waves’, the worst between April-June 2021 that overwhelmed our hospitals and killed an untold number of people. COVID19 primarily infects the respiratory system (the nasal passage, the wind-pipe and lungs), wrecking a lot of damage in people with underlying issues like diabetes or hypertension.
A lesser-known fact is that a COVID19 infection opens the path for other opportunistic infections. These can affect unrelated parts of the body—including the eye. Sometimes, tiny deficiencies in care combined with environmental factors compounds the risk of a COVID19-infected individual developing a vision-threatening eye condition: a corneal ulcer.
LVPEI’s team of ophthalmologists and researchers have been exploring the myriad sequelae of a COVID19 infection in the eye. On National Science Day, this post explores how a COVID19-infected individual’s circumstances can precipitate into a corneal ulcer (keratitis). It marks LVPEI’s contributions to the growing research around the world on the consequences of the pandemic on our health and well-being. Now, on to the cornea.
COVID19 and the Cornea
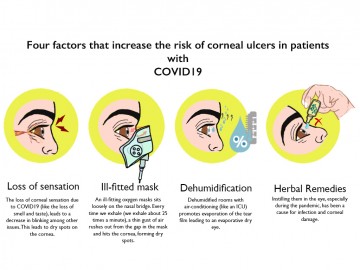
The relationship between COVID19 infection and the cornea remains under-explored, though research offers some tantalising clues. Keratitis or corneal ulcers are the primary cause of concern in people with a COVI19 infection, especially when they are hospitalised. A series of conditions layer together to form dry patches on the cornea, compounding the risk of a corneal ulcer. They are:
- Loss of sensation: A common symptom of a COVID19 infection is the temporary loss of smell and taste. For some, it can also lead to a temporary loss of corneal sensation. Nerves play a key role in keeping the cornea healthy, and this loss of sensation has various knock-on effects. The person may blink less, leading to a dry eye and the corneal epithelium breaks down leading to keratitis or inflammation.
- Ill-fitting oxygen masks: Many COVID19 patients needed supplemental oxygen. In some cases, they are given muscle-relaxants or sedatives, which makes their eyelids to droop—not fully close, that is. Then, an ill-fitting oxygen mask can blow exhaled air onto a patient’s eyes leading to dry patches on their corneas. As we exhale, on average, 25 times in a minute, the dry patch can lead to a corneal ulcer over time.
- Dehumidified places: Dehumidified rooms with air-conditioning (like an ICU) promotes evaporation of the tear film leading to an evaporative dry eye.
- Herbal remedies: The second wave saw a deluge of patients and a severe shortage of medical care. Many patients, desperate to save themselves or their loved ones, reached out to any care that was handy, including herbal remedies. Some patients applied ‘herbal drops’ to their eyes, which were contaminated, leading to corneal infections.
All these and myriad other factors point to probable causes of corneal ulcers during the pandemic—but we need to understand them better.
Herbal drops and a corneal infection: a story
Ramesh Punekar (name changed), 69 years old, caught COVID19 during the second wave. He was diabetic, hypertensive and had coronary heart disease. A few weeks after the infection, he began to have defective/impaired vision. Ramesh suffered for 9 months. Soon, both eyes became impaired. He sought multiple consultations and was prescribed, at different points, the gamut of ophthalmologic antimicrobial therapy--antifungals, antibiotics, topical and oral antivirals, and topical steroids.
When he finally made it to LVPEI, the consultants at LVPEI saw stromal infiltrate—a build-up of substances in the ocular tissue--deep into his cornea. Ramesh’s samples tested negative for fungi, Cytomegalovirus (CMV), Herpes simplex virus (HSV) and Varicella Zoster Virus (VZV).
Confocal microscopy finally revealed small hyper-reflective dots, strongly suggesting a stromal microsporidial infection. Microsporidia are tiny, unicellular parasites that form microscopic spores. They are an emerging cause of infectious disease.
The doctors interviewed Ramesh and his son who shared a history of herbal eye drop usage. Ramesh had COVID19-like symptoms along with his family just a few weeks prior to the onset of ocular symptoms.
After penetrating bilateral Keratoplasty—a corneal transplant--on both his eyes, Ramesh has some hope of regaining sight.
With contributions from Dr Muralidhar Ramappa, Faculty, the Cornea Institute.
Illustrated by Rupsy Khurana.