A new paper by Dr Niroj Kumar Sahoo and others from L V Prasad Eye Institute, Hyderabad; Narayana Nethralaya, Bengaluru and University of Pittsburgh, USA analyzes the post operative hole closure pattern in patients with idiopathic macular holes using ‘en face’ optical coherence tomography (OCT).
A macular hole is a central retinal defect and is often a product of age-related changes to the eye. It presents in the macula as a circular opening a few hundred microns in diameter and impairs central vision. A vitrectomy is the standard of care for macular holes. The procedure releases pressure on the macula and a gas bubble is used to flatten the hole and bring the tissue together, thereby aiding hole closure. A variety of factors can lead to a successful closure, including the orientation of the hole and its particular pattern of closure.
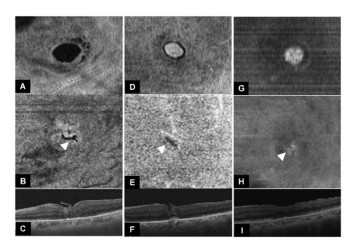
Optical coherence tomography (OCT) is the imaging tool used to identify and classify hole closure patterns on the macula. As the power and resolution of OCT technology improved over the decades, so has our ability to develop a nuanced classification of hole closure patterns in the eye. These OCT images are rendered as cross-sectional representations of the holes and their healing patterns. In fact, the current generation of OCTs enable ‘en face’ imaging: frontal images of specific retinal segments. This gives a new perspective of macular holes and their healing patterns, offering fresh insights into their morphology and prognosis.
A new paper in the Ophthalmology Retina by Dr Niroj Kumar Sahoo and others analyzes the post-operative closure patterns of full thickness macular holes using en face OCT. This retrospective study of 24 males and 40 females (64 eyes of 62 patients) measures the type of ‘en face’ hole closure and the final visual acuity achieved at 3 months. All the patients underwent vitrectomy along with ILM peeling, with or without ILM graft, over an 8-year period from January 2015 to 2022. Only holes that had achieved closure post-surgery were included in the study.
The authors described two types of hole closures: ‘round/indistinct’ and ‘linear’. They found that the orientation of the macular hole (its shape: circular, oval etc.) impacted the post-operative closure pattern. The distance between the margins mattered. Holes larger than 650 microns that closed linearly had a better final visual acuity at 3 months when compared to those with round/indistinct closure. Perhaps, the closer distance between margins aided in better closure and healing. This kind of insight is made possible by ‘en face’ OCT images as opposed to conventional cross-sectional ones—and this paper is one of the first to utilize it. The authors hope that their findings will enable larger studies in the future.
We previously used to use cross-sectional OCT to check the type of closure and tell the patient about the visual prognosis. In this paper, we demonstrated a 2-dimensional aspect of the closure. We discussed how the hole closed, and how that pattern relates to visual recovery. We plan to further study and assess what factors are responsible for these closure patterns which can be used for customizing macular hole surgery and to predict the amount of visual recovery,” says Dr Niroj Kumar Sahoo, corresponding author of the paper and Consultant Ophthalmologist, LVPEI.
Citation
Sahoo NK, Suresh A, Patil A, Ong J, Kazi E, Tyagi M, Narayanan R, Nayak S, Jacob N, Venkatesh R, Chhablani J. Novel en-face optical coherence tomography based closure patterns in idiopathic macular holes. Ophthalmol Retina.
Photo credit: Macular hole closures; Sahoo et al.