A new retrospective study by Dr Manjushree Bhate and others from the L V Prasad Eye Institute evaluates the clinical characteristics and the risk of vision impairment and exposure keratopathy in 112 children with Facial Nerve Palsy.
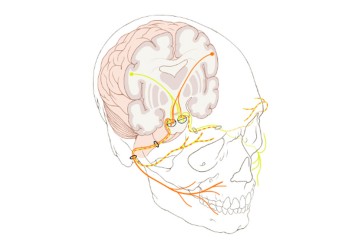
Facial Nerve Palsy (FNP) is a paralysis of the ‘Facial Nerve’ (Nerve 7 out of a set of 12 cranial nerves), so called as it innervates the muscles of the face. The paralysis of a sub-branch of the facial nerve also affects the functioning of the orbicularis muscle of the eye, compromising the eyelid’s ability to blink or close. Studies in adult populations have found that anywhere from 50%-80% of patients with FNP have dry eyes, and a smaller sub-set develop vision loss. In fact, the longer a person has FNP, the higher the risk of developing ‘lagophthalmos’, or the incomplete closure of eyelids. Another risk factor is the weakening of a defense reflex called ‘Bell’s phenomenon’, where the eyeball rolls the cornea up and away from the nose on blinking. The loss of all these reflexes exposes the cornea and dries it out, potentially leading to scarring. When multiple cranial nerves such as the 6th or 3rd nerves are palsied, the ability to converge or diverge eyeballs may be weakened as well, resulting in strabismus (squint).
Most cases of FNP are ‘idiopathic’; they arise spontaneously without any known cause. Sometimes, though, the cause could be a tumor, congenital anomalies, or even trauma. In most cases, FNP subsides on its own after a few days, though it can persist for months. FNP most commonly affects a single side of the face. Both men and women have an equal risk of developing FNP over their lifetime. Idiopathic FNP is relatively less common in children, as the incidence increases with age. While previous studies have characterized FNP in children, its ocular characteristics in a pediatric population remain under-explored and need better description.
In a new paper in the Journal of the American Association for Pediatric Ophthalmology and Strabismus, Drs Manjushree Bhate, Anthony Vipin Das and Swati Singh report on the ocular manifestations of FNP in a large cohort of paediatric patients. Their retrospective study included a cohort of 112 children (121 eyes) with a mean age of about 8 years. FNP presented roughly equally on either side of the face in this group and had a similar spread among both sexes (Male: 52%). Nearly two-thirds of cases were idiopathic, followed by congenital causes, and trauma. About 15% had multiple cranial nerve palsies.
One-fifth of the children (23; 20.5%) had moderate to severe vision loss and 43 children (38.4%) had ‘exposure keratopathy’, or corneal damage. Lagophthalmos was present in 70 eyes—and a big fraction (76.6%) of children with exposure keratopathy had lagophthalmos. A key finding of this study is that the presence of lagophthalmos was adequate to associate it with corneal damage; poor Bell’s phenomenon or other risk factors didn’t matter much in this paediatric cohort. While FNP affects both sexes, male children presented with a slightly higher distribution of vision impairment (55%) and ocular surface exposure (55.8%). The authors report that early management of lagophthalmos and eyelid retraction, though surgery may carry risk of amblyopia, will be crucial to preventing ocular complications of FNP in children.
‘While addressing the cause of facial nerve palsy is of paramount importance, preserving and protecting the surface of the eye and thereby maintaining the vision of the affected eye in a patient is crucial since this can avoid needless blindness,’ noted Dr Manjushree Bhate, Consultant Ophthalmologist, Child Sight Institute, LVPEI. ‘In situations where the involvement is severe or more than one cranial nerve is involved, multiple disciplines in medicine such as general medicine, ophthalmology, and neurology are required in patient care.’
Citation:
Bhate M, Das AV, Singh S. Characteristics of facial nerve palsy in 112 children and risk factors for ocular complications. J AAPOS. 2023 Jun;27(3):141.e1-141.e5. doi: 10.1016/j.jaapos.2023.03.003. Epub 2023 May 6. PMID: 37156335.
Photo credit: Cranial Nerve 7; Illustration by Patrick Lynch; CC BY 2.5.