In a new study from LVPEI, Drs. Swapna Shanbhag, Anahita Kate, and others assessed the long-term outcomes of autologous simple limbal epithelial transplant (SLET), which has revolutionized ocular surface restoration in patients with limbal stem cell deficiency (LSCD).
The cornea, the clear dome of the eye, is made of layers of transparent epithelium. The cornea repairs itself and maintains transparency using a reserve of stem cells in the limbus, a thin ring that separates the cornea from the whites of the eye (sclera). Severe damage to the cornea, such as due to chemical burns, can damage the limbus, permanently stripping the cornea of its regenerative ability—a condition called limbal stem cell deficiency (LSCD). Without the limbus, the cornea eventually breaks down, and cells from the conjunctiva—a thin cell layer that covers the sclera—envelop the cornea, blinding the eye. Such cases may require limbal stem cell transplantation.
Simple limbal epithelial transplantation (SLET) is a novel surgical technique described in 2012 at LVPEI. In cases of LSCD where only one eye is affected, limbal stem cells can be collected from the healthy eye, processed, and transplanted to the affected eye. Since the cells belong to the same person (autologous), systemic immunosuppression is not required. Autologous SLET showed promising results, with 76% of patients showing positive outcomes (improved visual acuity) over a 1.5-year period. SLET is more cost-effective and accessible than alternatives like the Cultivated Autologous Limbal Epithelial Cells (CALEC) technique. What we need is data on the long-term outcomes of autologous SLET to cement its reputation.
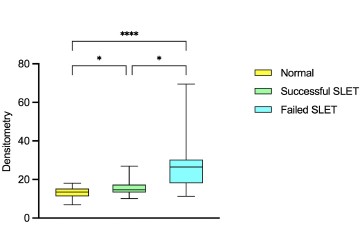
In a new study published in the American Journal of Ophthalmology, Drs. Swapna Shanbhag, Anahita Kate, and others from LVPEI report on just such long-term outcomes of SLET. They present an assessment of the corneal epithelium of 47 patients (94 eyes) 5-12 years (median: 5.75 years) after undergoing SLET. The patients had unilateral LSCD following chemical burns. Both eyes of each patient were examined using a variety of microscopic imaging techniques, such as slit lamp biomicroscopy and in vivo confocal microscopy. The researchers assessed whether SLET restored the cornea’s typical features, the corneal epithelial phenotype (CEP), normal corneal epithelial thickness (CET), corneal reflectivity, and transparency measured using densitometry. They found that while 32 (68%) eyes maintained a successful outcome, only 15 eyes had partial or total failure over this long follow-up period.
Multiple imaging techniques showed that CEP was normal in 68% of the limbal stem cell recipient eyes and all donor eyes. A healthy cornea is transparent and has low reflectivity. Injury or inflammation can lower the transparency, causing the cornea to reflect more light. A significant improvement was noted in these parameters in eyes that had successful outcomes after SLET. About 70% of the eyes that underwent SLET saw significant (over two lines on a chart) postoperative improvement in visual acuity. The study reveals that SLET has positive long-term outcomes in two-thirds of the cases. Moreover, changes in CEP, reflectivity, and densitometry are effective biomarkers of SLET’s efficacy.
‘Our findings highlight that SLET offers lasting restoration of the corneal surface, with good visual rehabilitation,’ says Dr. Anahita Kate, consultant ophthalmologist, LVPEI. ‘We also identified simple, non-invasive ways to monitor recovery after surgery, which can guide follow-up care for patients.’
‘This study is different from previously published studies on outcomes of limbal stem cell transplantation as we have shown quantitative outcomes on the basis of objective parameters with imaging techniques as opposed to only qualitative outcomes based on clinical evaluation, which was the norm in previous studies,’ notes Dr. Swapna Shanbhag, the first author of this study and a consultant ophthalmologist.
Citation
Shanbhag, S. S., Kate, A., Ganguly, S., Jakati, S., Deshmukh, R., & Basu, S. (2025). Five- to Twelve-Year Outcomes of Autologous Simple Limbal Epithelial Transplantation: Long-Term Corneal Epithelial Imaging and Phenotypic Analysis. American Journal of Ophthalmology, 273, 107–118. Advance online publication. >https://doi.org/10.1016/j.ajo.2025.02.003
Photo credit: Figure 7, box-and-whisker plot on epithelial densitometry; Shanbhag et al.