A review by Dr Vivek Singh and others, including from the University of Hyderabad, Manipal Academy of Higher Education, and the dept. of ophthalmology, Pius-hospital, Germany, discusses a range of emerging stem-cell, tissue engineering and regeneration therapies to tackle Dry Eye Disease caused by a dysfunctional lacrimal gland.
An estimated 344 million people are affected by Dry Eye Disease (DED) globally. A previous study from LVPEI warned that nearly 40% of the urban Indian population may have DED by 2030. A number of factors can cause this condition, which is characterized by the loss or instability of the tear film that protects and lubricates the ocular surface. Tear film is enriched with hundreds of proteins, electrolytes, and lipids, and is primarily made up of an aqueous fluid that is produced by a set of two lacrimal lobes in the eye. An impaired lacrimal gland can disrupt the tear film, leading to dehydration of the ocular surface by making it ‘aqueous-deficient’. Consequences of DED include corneal damage, and ultimately, even vision impairment and blindness.
DED is incurable. Current treatment strategies are palliative and cannot reverse the damage. These treatments range from pharmaceutical and biological tear substitutes, punctal plugs that stop tears from draining away, to corticosteroids to tackle any ocular surface inflammation. However, as DED progresses and becomes more acute, none of these therapies are adequate or effective. Groups around the world have been exploring a variety of emerging therapies, including stem-cell therapies, that are showing a lot of promise in restoring or regenerating a damaged lacrimal gland.
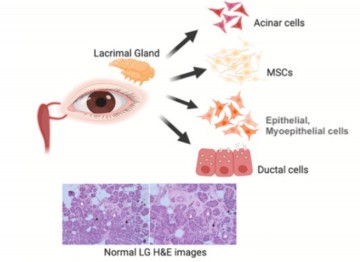
A new paper in The Ocular Surface by Dr Vivek Singh, Centre for Ocular Regeneration, LVPEI and others, explores the range of emerging therapies to regenerate the lacrimal gland. The paper is a comprehensive review of current strategies including lacrimal gland cell cultures, stem-cell therapies that cover progenitor cells, mesenchymal stromal cells, pluripotent and embryonic human stem cells, and finally, bioengineering and regeneration techniques. The paper’s many illustrations and tables are clear and well thought-through. They help understand specific approaches, the broad state of affairs, limitations, and the promise of clinical therapy that each of these therapies offer today.
While the paper notes the particular promise of stem cell therapies, it also explores a fully bioengineered and regenerated lacrimal gland, grown in a laboratory. To address the fundamental problem of immune rejection, decellularized (the process of isolating and removing cells from tissue, leaving behind collagen or other enzymes) tissue ‘scaffolds’ are repopulated with regenerated lacrimal cells. These approaches are on the frontiers of therapy, and the size and function of lacrimal glands makes them a prime target for such an approach. Together, all these therapies will be the key to addressing DED and offering treatment to the many millions who might need it.
‘The findings summarized in this review are the approaches that can be used for lacrimal gland regeneration in patients suffering from dry eye disease. Even though the studies are mostly in-vivo (in animals) and in-vitro (in a lab), these can be helpful to understand the regenerative mechanisms behind the cell-based therapies to treat DED,’ says Dr Vivek Singh, the corresponding author of this paper and Scientist, Sudhakar and Sreekanth Ravi Stem Cell Biology Laboratory, LVPEI.
Citation
Veernala I, Jaffet J, Fried J, Mertsch S, Schrader S, Basu S, Vemuganti GK, Singh V. Lacrimal gland regeneration: The unmet challenges and promise for dry eye therapy. Ocul Surf. 2022 Jul;25:129-141. doi: 10.1016/j.jtos.2022.06.005. Epub 2022 Jun 23. PMID: 35753665.
Photo credit: Fig.1 Schematic diagram of the lacrimal gland and its inherent cells, and H&E image, credit: Veernala I et al.