In this case series, Drs. Deepika C. Parameswarappa, Sirisha Senthil, and others from LVPEI, described how pathogenic mutations in the BEST1 gene causing bestrophinopathies, a spectrum of inherited retinal diseases, is associated with very severe, potentially blinding, angle-closure glaucoma in young patients.
Bestrophin 1 belongs to an ancient class of (cell) membrane proteins that is expressed primarily in the retina, the innermost layer of the eye, and encoded by the BEST1 gene. Any pathogenic mutation in the gene can lead to bestrophinopathies, a spectrum of five hereditary eye disorders that degenerate the retina, resulting in blindness. Best vitelliform macular dystrophy (BVMD) and autosomal recessive bestrophinopathy (ARB) are the two most common forms of these disorders. These mutations halt the production of the bestrophin-1 protein in the retinal pigment epithelium, a layer of cells that nourishes the retina, resulting in retinal degeneration. There are no known treatments for bestrophinopathies. To make matters worse, young patients with bestrophinopathy can develop angle closure glaucoma, which can lead to blindness without early detection and proper treatment.
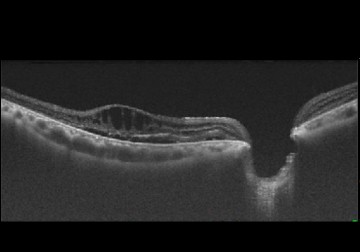
Angle-closure glaucoma (ACG) happens when the front part of the eye gets narrow due to a lack of space, which blocks intraocular fluids from draining out, raising the pressure inside the eye that in turn damages the optic nerve. Patients with bestrophinopathies are at very high risk of developing ACG. A majority do not respond to eye drops and laser and will need surgery. Most types of glaucoma surgery in these patients trigger a serious intraoperative and postoperative blinding complication called malignant glaucoma or aqueous misdirection syndrome.
In a new case series published in the journal Ophthalmic Genetics, Drs. Deepika C. Parameswarappa, Sirisha Senthil, and others from LVPEI, described how mutations in the BEST1 gene associate two bestrophinopathies, ARB and BVMD, with unresponsive angle closure glaucoma and post-surgical malignant glaucoma present and behave. The paper describes six cases, five patients with ARB (cases 1-4 and 6) and one with BVMD (case 5). All six patients had ACG and required surgery (except case 4) for their uncontrolled glaucoma. All five patients who underwent glaucoma surgery developed MG. Only surgical removal of the vitreous (the gel-like substance in our eyes), and making a fluid drainage pathway within the eye (from posterior to anterior segments) helped to reduce intraocular pressure in patients with MG.
Next generation sequencing revealed autosomal recessive pattern of inheritance (inherited when both parents were carriers) and one patient had an autosomal dominant pattern of inheritance of bestrophinopathy. Hence it is important for the family members (siblings, children and grandchildren) of these patients to be evaluated for similar conditions. Notably, the retinal problems manifested before patients developed glaucoma.
Dr. Sirisha Senthil, Head of the VST Centre for Glaucoma and the corresponding author for this paper, noted that patients, 'need to be educated about regular eye checkups for both retina and glaucoma for early diagnosis and intervention in patients with bestrophinopathy. While these conditions cannot be completely cured, the glaucoma in these eyes will need a different approach compared to conventional methods.' She notes that the doctors at LVPEI have devised safer methods to treat this condition and prevent blinding complications like malignant glaucoma.
Citation
Parameswarappa, D. C., Balasubramnian, J., Kumar Padhy, S., Hansraj, S., Natarajan, R., Kannabiran, C., Garudadri, C., & Senthil, S. (2024). BEST1 associated bestrophinopathies with angle closure and post-surgical malignant glaucoma. Ophthalmic Genetics, 1–12. Advance online publication. https://doi.org/10.1080/13816810.2024.2398827